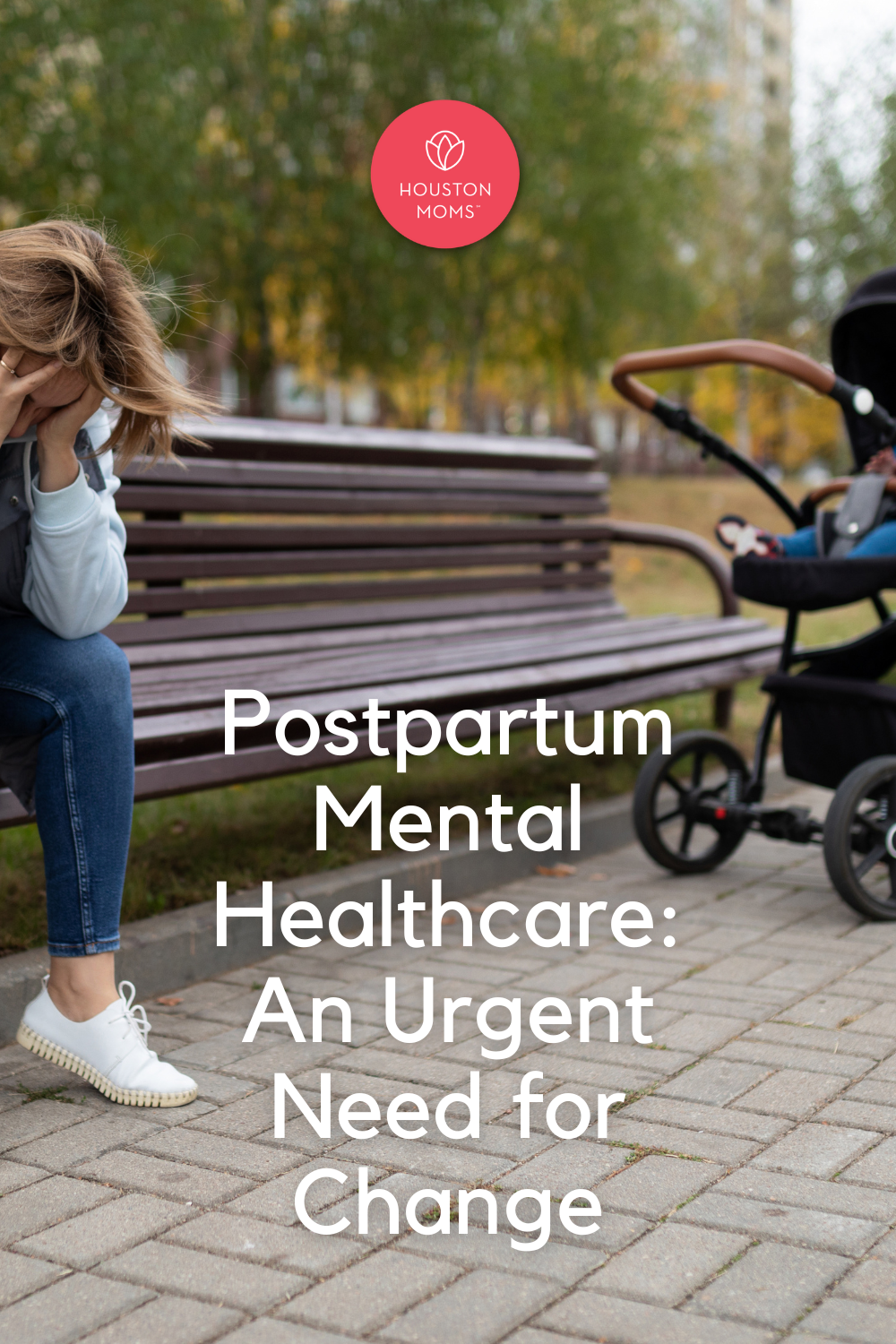
When I read about Lindsay Clancy and her three precious babies, my heart broke. Now, my soul literally aches for her and her family as the latest victims of our nation’s horrible lack of mental healthcare. As further details emerge about what happened that day and the previous months leading up to it, there are going to be many opinions on Lindsay’s state of mind. I imagine it will turn into a battle of doctors and expert witnesses in the
courtroom. However, I am still certain that this happened because of inadequate resources and medical treatment available to Lindsay when she needed help with her mental illness. Postpartum depression (PPD) is real; it does not discriminate and affects about 1 in 8 of new mothers. Lindsay Clancy most likely suffered from Postpartum Psychosis, which is far rarer. Postpartum Psychosis is often characterized by hallucinations and delusions.
 Seeking Mental Healthcare for PPD
Seeking Mental Healthcare for PPD
I am lucky enough to not be able to compare my experience with PPD to Lindsay’s story, but it was still very scary. My son Lucas was 3 months old when I returned to work after my maternity leave. I struggled to find a routine with an infant and working 24-hour shifts. I was plagued with anxiety about pumping at work with an unpredictable schedule and my milk supply tanked almost immediately. I was exhausted, had a lot of crying spells, and nearly constant feelings of guilt about being a bad mother and wife. All of this continued to spiral downward over the next several months. The hot Houston weather had returned, keeping us trapped indoors during the day and my mind was plagued with anxiety and depression, including thoughts of suicide.
I never had thoughts of hurting Lucas, but I knew I needed help before things got even worse. Because I had experienced an episode of major depression during college, I knew the symptoms and that I was starting to spiral downward. I called my OB for a referral and his nurse told me that with my discharge instructions from the hospital, there was a blue piece of paper that had a list of therapists, psychiatrists and other resources for PPD. Luckily, I still had it. I remember feeling so tired and defeated as I started calling the numbers on the list. The first person had a voicemail- I left what was most likely a garbled message through my tears and never got a call back.
The next therapist I reached didn’t have an opening for three weeks. No, I needed help now. I finally found a psychiatrist who could see me that week, but her fee was $350 and she didn’t accept insurance. I would call back after discussing it with my husband, I said. That was a lot of money for us with me just being out of work with unpaid maternity leave. I felt as though I had nowhere to turn and it had taken all of my energy that day just to make those phone calls.
Help that Wasn’t Helpful
I considered going to the ER, but knew from nursing experience, that I would only be separated from Lucas and put in a unit with patients who had a wide range of diagnoses from depression to schizophrenia. That would probably just make me feel worse, even if it was a safe place. I even tried urgent care at one point, only to be turned away and referred to a hospital. I worked up the energy one day to attend a support group for PPD with other moms. I left only feeling worse about myself…..the leader had told us all to each look at our baby and feel grateful for their health. After all, she said, things could be much worse…..you could have a sick baby in the NICU. That statement only made me feel more shame and guilt.
Navigating a Second Pregnancy
After much desperation, I was lucky enough to find help through the reproductive psychiatry office at Texas Children’s Hospital. I am guessing that this option wasn’t included on the blue sheet of resources because Texas Children’s is a big competitor of the hospital where I delivered Lucas. I was treated by a psychiatrist there for a few years as I worked hard to get my mental state back on track. I continued to seek their help as we navigated the stressful path of IVF for our second child. I eventually also found a wonderful therapist who helped immensely.
Even though I was kept on an antidepressant through my pregnancy with Ellie and informed the hospital staff of my history with postpartum depression, not once was I asked about it or screened during my long hospitalization with her. Upon discharge, no one ever addressed postpartum depression and the same exact blue sheet was included in my discharge paperwork. I don’t even think it had been updated. I was informed, however, that all support groups were suspended due to COVID.
I still struggled with my mental health after having Ellie, but I felt better prepared with a doctor and a therapist who were already managing my care through telehealth. I also knew that I would not be able to manage a full time job and a new baby this time around. Luckily, my symptoms were not as severe, but I did experience a lot of isolation and loneliness brought on by COVID.
Maternal Mental Healthcare Needs to Change
 I am telling you my story because this needs to change. If this was my experience trying to find help, I can’t imagine a new mom with little support and no resources trying to access mental healthcare. The United States has the highest rate of maternal mortality of all high-income countries. In the CDC’s most recent report, mental health conditions are the overall most frequent cause of pregnancy-related deaths. Approximately 23% of deaths are attributed to suicide, substance use disorder, or are otherwise associated with a mental health condition.
I am telling you my story because this needs to change. If this was my experience trying to find help, I can’t imagine a new mom with little support and no resources trying to access mental healthcare. The United States has the highest rate of maternal mortality of all high-income countries. In the CDC’s most recent report, mental health conditions are the overall most frequent cause of pregnancy-related deaths. Approximately 23% of deaths are attributed to suicide, substance use disorder, or are otherwise associated with a mental health condition.
It is a passion of mine to help develop a program in Houston to help struggling moms who desperately need help for PPD immediately, not in three weeks. A program that addresses the unique needs of the disease and recognizes that there is also an infant involved. One that accepts insurance and is accessible to all new mothers regardless of income. Although I am grateful to the reproductive psychiatry office and doctor where I found help, they were only there from 8-5 and only offered me one appointment a week. Once Ellie is in school, I plan to make it my mission to do what I can as an individual and hopefully with help as a team to create a place where moms with PPD and associated mental disorders can go. In the meantime, all I can do is share my story for better awareness and to be a listening ear and resource for anyone who needs help and doesn’t know how to get it.
My wish for Lindsay Clancy is that she is getting the help that she needs and that through education and awareness, the world won’t see her as a monster who murdered her children, but as a loving mother who was ill and couldn’t get the healing she needed from our lack of appropriate mental healthcare.
 About Kari Hull
About Kari Hull
Kari is a former Labor and Delivery RN and high risk OB Flight RN. She now stays at home with Lucas (9) and Ellie (2).